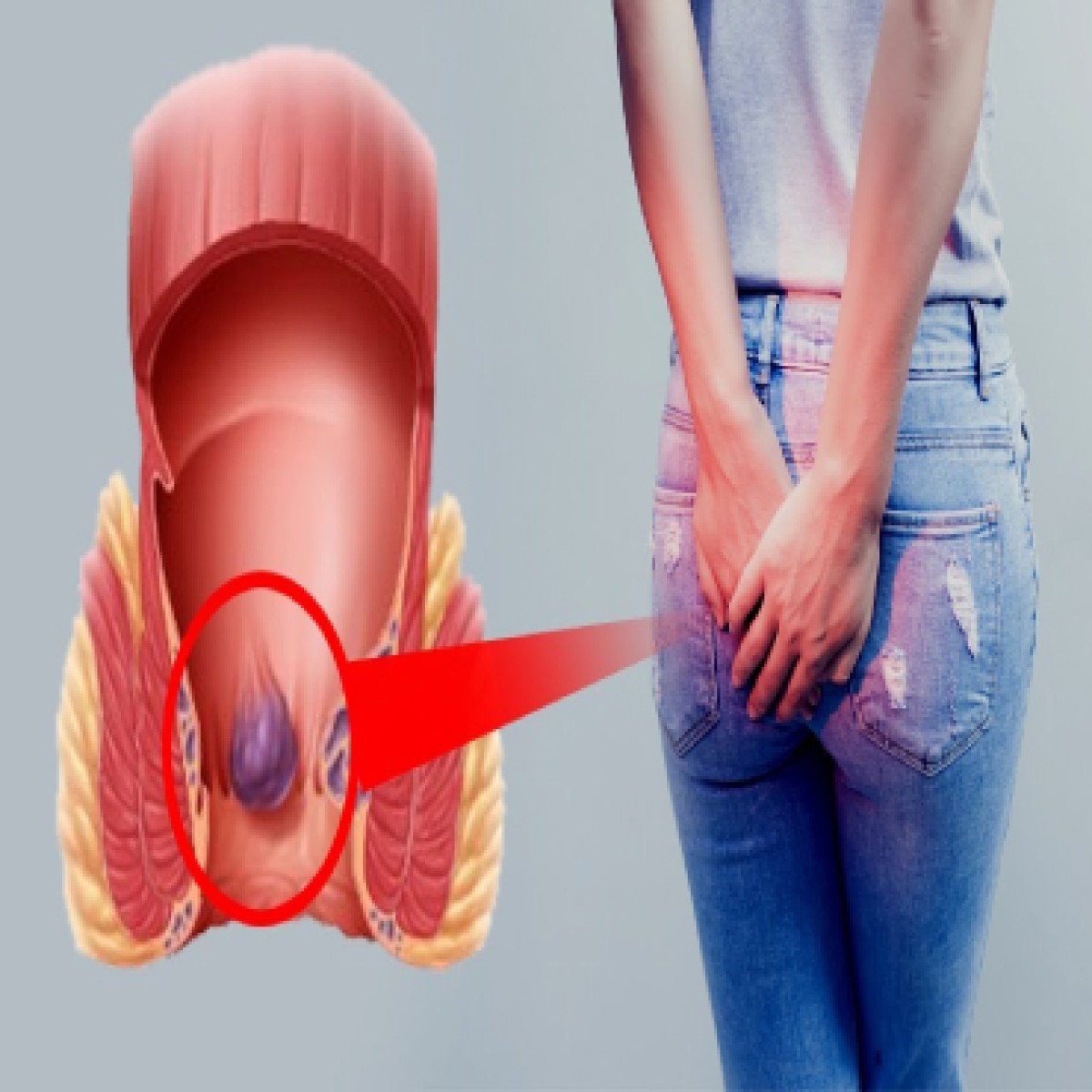
What are piles?
Piles are inflamed and swollen collections of tissue in the anal area. They can have a range of sizes, and they may be internal or external. Internal piles are normally located between 2 and 4 centimeters (cm) above the opening of the anus, and they are the more common type. External hemorrhoids or External piles occur on the outside edge of the anus. Internal hemorrhoids are so far inside your rectum that you can't usually see or feel them. They don't generally hurt because you have few pain-sensing nerves there.
Piles is classified into four grades:
1. Grade I: There are small inflammations, usually inside the lining of the anus. They are not visible.
2. Grade II: Grade II piles are larger than grade I piles, but also remain inside the anus. They may get pushed out during the passing of stool, but they will return unaided.
3. Grade III: These are also known as prolapsed hemorrhoids, and appear outside the anus. The individual may feel them hanging from the rectum, but they can be easily re-inserted.
4. Grade IV: These cannot be pushed back in and need treatment. They are large and remain outside of the anus
Piles are inflamed and swollen collections of tissue in the anal area. They can have a range of sizes, and they may be internal or external. Internal piles are normally located between 2 and 4 centimeters (cm) above the opening of the anus, and they are the more common type. External hemorrhoids or External piles occur on the outside edge of the anus. Internal hemorrhoids are so far inside your rectum that you can't usually see or feel them. They don't generally hurt because you have few pain-sensing nerves there.
Piles is classified into four grades:
1. Grade I: There are small inflammations, usually inside the lining of the anus. They are not visible.
2. Grade II: Grade II piles are larger than grade I piles, but also remain inside the anus. They may get pushed out during the passing of stool, but they will return unaided.
3. Grade III: These are also known as prolapsed hemorrhoids, and appear outside the anus. The individual may feel them hanging from the rectum, but they can be easily re-inserted.
4. Grade IV: These cannot be pushed back in and need treatment. They are large and remain outside of the anus
Signs and Symptoms
In most cases, the symptoms of piles are not serious. They normally resolve on their own after a few days. An individual with piles may experience the following symptoms:
- A hard, possibly painful lump may be felt around the anus. It may contain coagulated blood. Piles that contain blood are called thrombosed external hemorrhoids.
- After passing a stool, a person with piles may experience the feeling that the bowels are still full.
- Bright red blood is visible after a bowel movement.
- The area around the anus is itchy, red, and sore.
- Pain occurs during the passing of a stool.
Piles can escalate into a more severe condition. This can include:
- excessive anal bleeding, also possibly leading to anemia
- infection
- fecal incontinence, or an inability to control bowel movements
- anal fistula, in which a new channel is created between the surface of the skin near the anus and the inside of the anus
- a strangulated hemorrhoid, in which the blood supply to the hemorrhoid is cut off, causing complications including infection or a blood clot
If any of the symptoms persists medical advice with proctologist will be helpful based on the grade medical or surgical treatment can be advised.
In most cases, the symptoms of piles are not serious. They normally resolve on their own after a few days. An individual with piles may experience the following symptoms:
- A hard, possibly painful lump may be felt around the anus. It may contain coagulated blood. Piles that contain blood are called thrombosed external hemorrhoids.
- After passing a stool, a person with piles may experience the feeling that the bowels are still full.
- Bright red blood is visible after a bowel movement.
- The area around the anus is itchy, red, and sore.
- Pain occurs during the passing of a stool.
Piles can escalate into a more severe condition. This can include:
- excessive anal bleeding, also possibly leading to anemia
- infection
- fecal incontinence, or an inability to control bowel movements
- anal fistula, in which a new channel is created between the surface of the skin near the anus and the inside of the anus
- a strangulated hemorrhoid, in which the blood supply to the hemorrhoid is cut off, causing complications including infection or a blood clot
If any of the symptoms persists medical advice with proctologist will be helpful based on the grade medical or surgical treatment can be advised.
Causes
Piles are caused by increased pressure in the lower rectum. The blood vessels around the anus and in the rectum will stretch under pressure and may swell or bulge, forming piles. This may be due to:
- Chronic constipation
- Chronic diarrhea
- Lifting heavy weights
- Pregnancy
- Straining when passing a stool
- Obesity
- Colon cancer
- Spinal cord injury
Piles are caused by increased pressure in the lower rectum. The blood vessels around the anus and in the rectum will stretch under pressure and may swell or bulge, forming piles. This may be due to:
- Chronic constipation
- Chronic diarrhea
- Lifting heavy weights
- Pregnancy
- Straining when passing a stool
- Obesity
- Colon cancer
- Spinal cord injury
Treatments
In the majority of cases, piles resolve on their own without the need for any treatment. However, some treatments can help significantly reduce the discomfort and itching that many people experience with piles.
- Lifestyle changes: We will initially recommend some lifestyle changes to manage piles.
- Diet: A change in diet can help keep the stools regular and soft. This involves eating more fiber, such as fruit and vegetables, or primarily eating bran-based breakfast cereals.
- Body weight: Losing weight may help reduce the incidence and severity of piles. Exercising is one of the main therapies for piles.
In the majority of cases, piles resolve on their own without the need for any treatment. However, some treatments can help significantly reduce the discomfort and itching that many people experience with piles.
- Lifestyle changes: We will initially recommend some lifestyle changes to manage piles.
- Diet: A change in diet can help keep the stools regular and soft. This involves eating more fiber, such as fruit and vegetables, or primarily eating bran-based breakfast cereals.
- Body weight: Losing weight may help reduce the incidence and severity of piles. Exercising is one of the main therapies for piles.
Medications
Several medicinal options are available to make symptoms more manageable for an individual with piles.
- OTC medications: These are available, including painkillers, ointments, creams, and pads, and can help soothe redness and swelling around the anus. Do not use them for more than 7 days in a row
- Laxatives: The doctor may prescribe laxatives if a person with piles suffers from constipation. These can help the person pass stools more easily and reduce pressure on the lower colon.
Several medicinal options are available to make symptoms more manageable for an individual with piles.
- OTC medications: These are available, including painkillers, ointments, creams, and pads, and can help soothe redness and swelling around the anus. Do not use them for more than 7 days in a row
- Laxatives: The doctor may prescribe laxatives if a person with piles suffers from constipation. These can help the person pass stools more easily and reduce pressure on the lower colon.
Surgical options
Advanced Piles require surgical treatment.
- Hemorrhoidectomy: The excess tissue that is causing the bleeding is surgically removed. This can be done in various ways.
- Banding: An elastic band around the base of the pile, cutting off its blood supply. After a few days, the hemorrhoid falls off. This is effective for treating all hemorrhoids of less than grade IV status.
- Stapled hemorrhoidopexy or Hemorrhoid stapling: Blood flow is blocked to the hemorrhoid tissue. It is a surgical procedure that involves the cutting and removal of Anal Hemorhoidal Vascular Cushion whose function is to help to seal stools and create continence. This procedure is usually less painful than hemorrhoidectomy.
- Sclerotherapy: Medicine is injected to make the hemorrhoid shrink. The hemorrhoid eventually shrivels up. This is effective for grade II and III hemorrhoids and is an alternative to banding.
- Haemorrhoidal artery ligation reduces the blood flow to haemorrhoids, with the aim of reducing discomfort and bleeding. It also aims to achieve some shrinkage of haemorrhoids but adjunctive treatment is required for large prolapsing haemorrhoids.
Advanced Piles require surgical treatment.
- Hemorrhoidectomy: The excess tissue that is causing the bleeding is surgically removed. This can be done in various ways.
- Banding: An elastic band around the base of the pile, cutting off its blood supply. After a few days, the hemorrhoid falls off. This is effective for treating all hemorrhoids of less than grade IV status.
- Stapled hemorrhoidopexy or Hemorrhoid stapling: Blood flow is blocked to the hemorrhoid tissue. It is a surgical procedure that involves the cutting and removal of Anal Hemorhoidal Vascular Cushion whose function is to help to seal stools and create continence. This procedure is usually less painful than hemorrhoidectomy.
- Sclerotherapy: Medicine is injected to make the hemorrhoid shrink. The hemorrhoid eventually shrivels up. This is effective for grade II and III hemorrhoids and is an alternative to banding.
- Haemorrhoidal artery ligation reduces the blood flow to haemorrhoids, with the aim of reducing discomfort and bleeding. It also aims to achieve some shrinkage of haemorrhoids but adjunctive treatment is required for large prolapsing haemorrhoids.



Leave a reply
Your email address will not be published.